Why You Still Don't Feel Like Yourself Since Becoming a Mom (And Why Biology Says That's Okay)
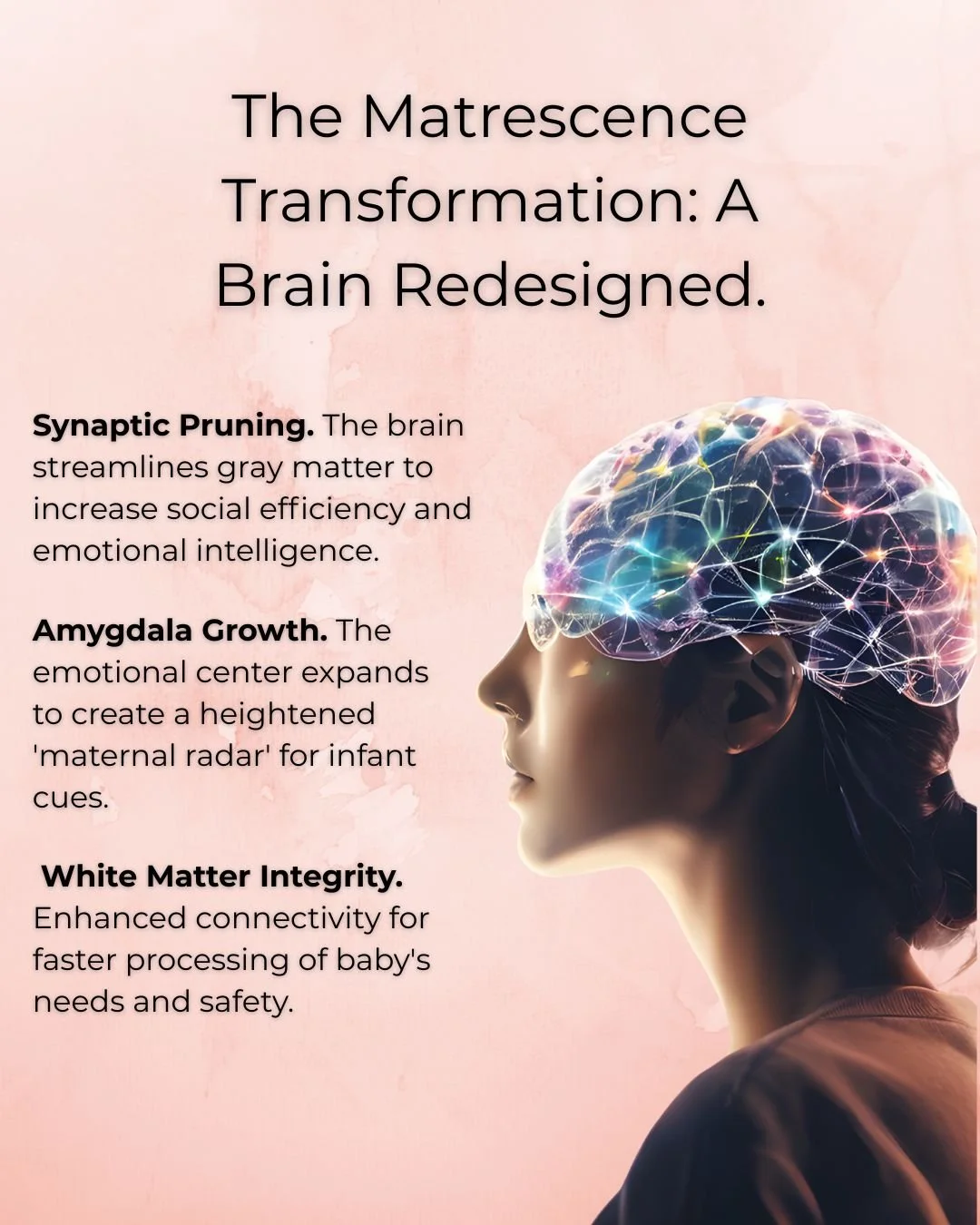
Motherhood triggers a profound developmental transition called matrescence, which involves actual structural changes in the brain. Your amygdala becomes more sensitive, your brain prunes neural pathways to increase attunement to your child, and your nervous system now processes your child's distress as if it were your own physical threat. This isn't weakness, it's measurable, biological change that fundamentally alters how you experience the world and shrinks your capacity for other stressors.
You had a baby a year ago, and you still don't feel like your old self. As you scroll through social media, your friends seem to have bounced back effortlessly,happy photos at apple orchards, mirror selfies from their morning workouts, glowing captions about how motherhood "completed" them.
Meanwhile, you're looking at your kitchen that's been in a state of collapse since... you can't even remember. Your baby still isn't sleeping through the night consistently. You've made it to exactly one exercise class this month, and you felt guilty the entire time for leaving. You're exhausted in a way that sleep doesn't fix.
And the question keeps coming: "What's wrong with me? Why can't I just get it together like everyone else?"
As a Registered Clinical Counsellor (RCC) and Occupational Therapist (OTR/L) with over 14 years of clinical experience working with families in Vancouver, British Columbia, I've sat with hundreds of parents in this exact moment. I specialize in nervous system regulation and parental burnout, using an integrated approach that combines attachment-based counseling with sensory-informed occupational therapy. And I need you to hear this: What you're experiencing isn't weakness, and it's not a parenting failure.
Your brain has literally reorganized itself since becoming a parent. This reorganization, called matrescence, makes you hyper-aware of your child's emotional state while simultaneously shrinking your capacity to manage your own needs. Research published in Nature Neuroscience found that pregnancy leads to significant gray matter reductions in regions involved in social cognition,changes that persist for at least two years postpartum. These aren't losses of function but rather neural specialization for the demanding work of motherhood.
Those friends on social media? They're either further along in the transition, have more support than you realize, or are posting their highlight reel while feeling exactly like you do behind the scenes.
The messy kitchen isn't the problem. The missed workouts aren't the problem. The problem is that you're trying to run your pre-baby life with a completely different nervous system, and no one told you that was going to happen. You’re doing the best you can with what you have and none of this is your fault.
Key Takeaways:
Matrescence involves measurable brain changes that increase emotional sensitivity and attunement
Your nervous system capacity shrinks because you're running constant background vigilance
Stress responses that revert to old patterns are biological, not character flaws
Recovery requires both rest AND reduced demands
Professional support for nervous system regulation can help rebuild sustainable capacity
In this post, we'll explore what matrescence is and why it makes your nervous system feel so raw, how your capacity shrinks in ways you didn't expect, and why you might find yourself reacting in ways that surprise you. You'll learn that what you're experiencing is a profound biological transition, not personal inadequacy.
You're not doing it wrong. You're doing something incredibly hard with a nervous system that's working overtime to keep everyone safe. And no, you don't need to "bounce back." You need to understand that you've become someone new.
What is matrescence and why does my nervous system feel so raw?
Matrescence is the profound developmental transition into motherhood that involves actual brain rewiring. Your amygdala (threat detection center) becomes more sensitive, your brain prunes neural pathways to increase attunement to your child, and your nervous system now processes your child's distress as if it were your own physical threat. This isn't metaphorical. It's measurable, biological change that fundamentally alters how you experience the world.
Your Brain Reorganizes to Hold Two Nervous Systems
Your nervous system didn't just add new responsibilities when you became a parent. It grew new rooms to hold your child's experience alongside your own. The problem? The walls between these rooms are thin. Your child's distress moves through you before you can even think about it.
This isn't metaphorical. Brain imaging studies show that a mother's amygdala lights up in response to her baby's cry before the prefrontal cortex (the thinking brain) even comes online. Research from the National Institutes of Health demonstrates that mothers' brains respond to their infant's cries with activation in regions associated with emotional processing and motor planning within milliseconds. Faster than conscious thought. Your body responds to your child's need as if it were a direct threat to your own safety.
Think of it like this: Before you became a parent, your nervous system was a container designed to hold your own experiences. Your emotions, your stress, your needs. The container had a certain size and capacity.
Now, that container has expanded to hold both your emotional world and your child's. You're not just feeling your own stress about the messy kitchen. You're also holding your child's disappointment about bedtime, their frustration about tomorrow's schedule, their big feelings about everything.
The attunement that makes you such a responsive, caring parent is the same mechanism that leaves you feeling overwhelmed and raw. Your nervous system is doing exactly what it evolved to do: prioritize your child's survival by making you exquisitely sensitive to their needs.
Why Small Things Feel Like Big Threats
When you're in this state of heightened sensitivity, your child's refusal to wear shoes can genuinely feel like an emergency. Not because you're dramatic or overreacting, but because your brain is interpreting their distress as danger.
I worked with a mother who described feeling "electrified" every time her toddler cried. Not angry. Just flooded. Her entire body would tense, her heart would race, and she'd feel an urgent need to make the crying stop immediately.
When we mapped her nervous system response, we discovered her heart rate jumped 20 beats per minute within seconds of her child's first whimper. Before she could even think "my child is crying," her body was already in a stress response.
This is your body doing exactly what it was designed to do: keep your child safe through hypervigilance. The cost is that you're constantly on alert, even when there's no actual danger. Your smoke detector is so sensitive that it goes off when you make toast.
The Biological Reality of Brain Rewiring
Let's talk about what's actually happening in your brain, because understanding the biology can help you stop blaming yourself.
During pregnancy and the postpartum period, your brain undergoes what neuroscientists call "synaptic pruning." Your brain is literally reorganizing its neural pathways, strengthening some connections and eliminating others.
The connections that get strengthened? The ones related to:
Reading your baby's cues
Responding to distress signals
Anticipating needs
Maintaining vigilance for threats
The connections that often get weakened? The ones related to:
Your own needs and preferences
Activities unrelated to caregiving
Previous identities and interests
Self-focused awareness
This isn't a character flaw or poor time management. This is your brain reorganizing to prioritize your child's survival. From an evolutionary perspective, this makes perfect sense. From a lived experience perspective, it can feel like you've lost yourself.
A landmark 2016 study published in Nature Neuroscience tracked first-time mothers for two years and found such significant and consistent changes in gray matter that researchers could identify which women had given birth based on brain scans alone. These changes persisted for at least two years after birth.
Matrescence vs. Postpartum Depression
It's important to distinguish between the normal overwhelm of matrescence and clinical postpartum depression or anxiety.
Matrescence is a developmental transition. It includes hard moments, exhaustion, identity shifts, and feeling overwhelmed. But it also includes moments of connection, joy, and feeling okay. The hard feelings come and go.
Postpartum depression is persistent. It doesn't lift with rest. If you're experiencing hopelessness that lasts most of the day, intrusive thoughts about harm, difficulty bonding with your baby, or thoughts of harming yourself, please reach out to a perinatal mental health specialist. In British Columbia, you can find support through the BC Reproductive Mental Health Program or by searching for a Registered Clinical Counsellor (RCC) who specializes in perinatal mental health. These symptoms are not just matrescence. They require professional support, and help is available.
How does matrescence shrink my capacity for everything else?
Before you became a parent, your nervous system had a certain bandwidth. You could handle work stress, relationship challenges, household tasks, and still have energy left over for yourself. Now, a baseline level of vigilance runs in the background at all times, using energy constantly. This means your capacity for other stressors has genuinely shrunk. Not because you've gotten weaker, but because you're already using so much bandwidth just to stay attuned.
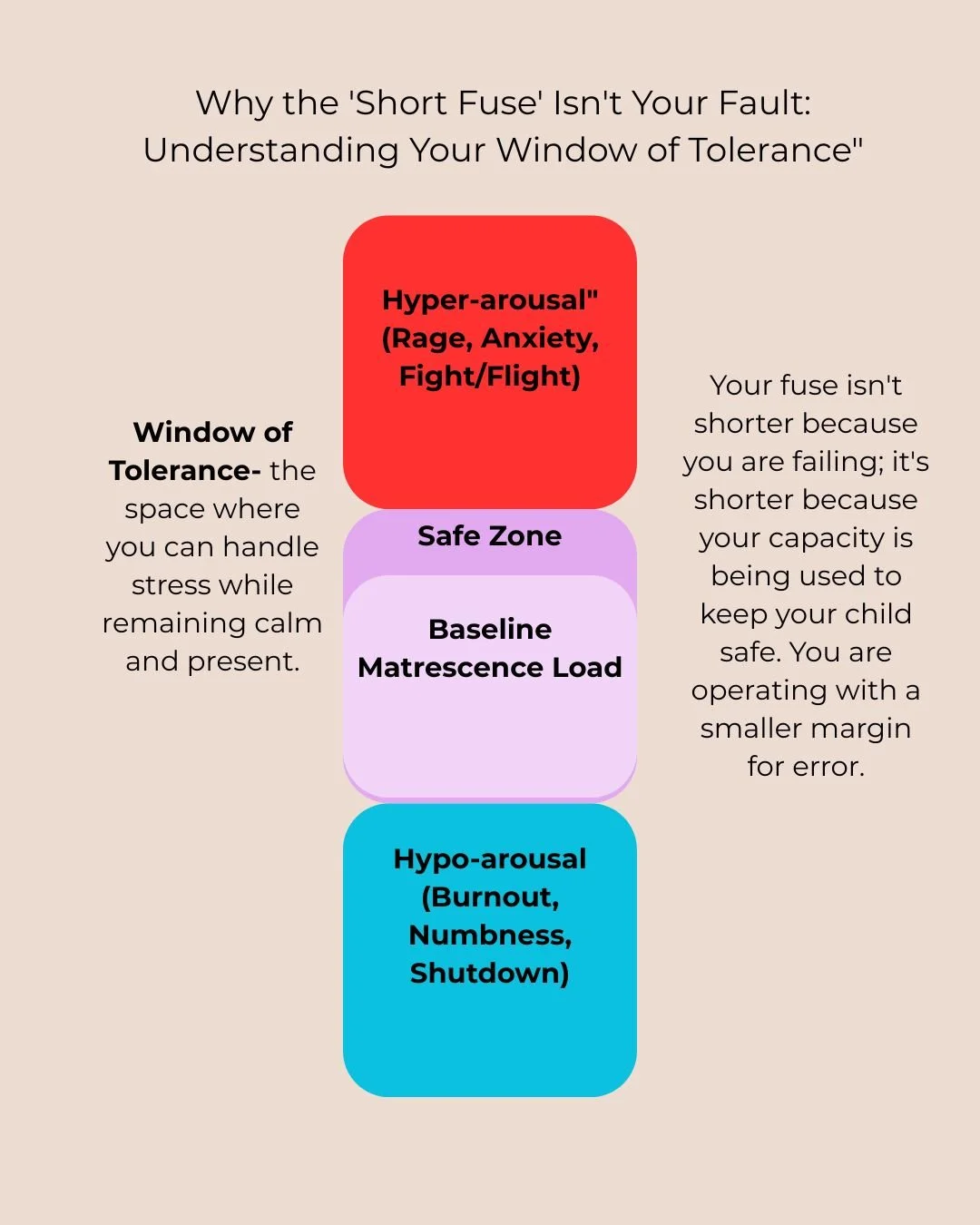
Understanding Your Window of Tolerance
In nervous system language, we talk about something called your Window of Tolerance. This concept, developed by Dr. Dan Siegel in his work on interpersonal neurobiology, refers to the range within which you can handle stress and still function well.
When you're inside your window:
You can think clearly and make decisions
You can manage your emotions
You respond to stress proportionally
You can access your coping skills
When stress pushes you outside your window, you tip into either:
Hyperarousal (fight or flight): anxiety, anger, racing thoughts, feeling overwhelmed
Hypoarousal (shutdown): numbness, brain fog, dissociation, wanting to escape
Before you became a parent, your window might have been wide. You could handle a stressful work deadline, a disagreement with your partner, a flat tire, and unexpected guests all in the same week and still feel relatively okay.
Matrescence narrows that window significantly.
Now, the background vigilance of tracking your child's well-being is already taking up space in your window. Add a sleepless night, your toddler refusing to get dressed, and burnt toast, and suddenly you're snapping at your partner or crying in the bathroom.
It's not that you've become fragile. It's that your baseline stress level is higher, so there's less room before you hit your limit.
The Invisible Mental Load
Even when your child is at school or asleep, part of your nervous system is still tracking their well-being. This background process uses energy. Real, measurable energy.
You might find yourself:
Mentally running through the schedule (pickup times, permission slips, what's in the fridge for dinner)
Monitoring for sounds (is that a cough? did they just wake up?)
Anticipating needs (we're almost out of milk, I need to remember to...)
Carrying emotional information (they seemed sad at drop-off, I wonder if...)
This mental load isn't just "remembering things." It's your nervous system maintaining a constant awareness of your child's state and needs, even when they're not physically present.
For neurodivergent parents, especially those with ADHD, this mental load is even more demanding. The executive function required to manage this invisible tracking while also managing your own life can push you into overwhelm faster.
Why You Can't Just "Push Through" Anymore
Before matrescence, you might have been able to function on less sleep, skip meals, work through stress, and generally push your body beyond its comfortable limits when needed.
Now, when you try to push through, your body rebels more quickly. You might notice:
Getting sick more often
Feeling exhausted even after sleep
Difficulty concentrating or making decisions
Physical tension that won't release
Emotional reactions that feel out of proportion
This isn't weakness. This is your nervous system telling you that it's already operating at near-capacity just to maintain baseline functioning. There's no reserve left for pushing through.
I've worked with many parents who feel frustrated by what they perceive as their decreased resilience. They remember being able to handle so much more before they had children, and they judge themselves harshly for their current limitations.
But you're not less resilient. You're using most of your resilience just to show up every day with a nervous system that's been fundamentally reorganized to prioritize another human being over yourself.
Why do I sometimes react in ways I swore I never would?
Under high stress, especially when you're beyond your Window of Tolerance, your brain loses access to the prefrontal cortex and reaches for the most deeply grooved neural pathways. Which are often the parenting patterns you witnessed as a child. This isn't a character flaw or moral failing. It's how the brain conserves energy during overwhelm. The good news: awareness is the first step to creating new pathways.
Your Brain's Default Settings Under Stress
When you're at capacity and your nervous system is overwhelmed, something predictable happens: your brain can't afford the energy required for conscious, intentional decision-making. So it runs the default program. The deeply grooved neural pathway created by the parenting you received.
Here's what's happening neurologically:
Under stress, blood flow to your prefrontal cortex (the part of your brain responsible for conscious choice, values-based decision-making, emotional regulation, and perspective-taking) decreases significantly.
Your brain stem and limbic system take over. These older, more primitive parts of your brain are focused solely on survival. They don't have access to the parenting books you've read, the gentle techniques you've learned, or the parent you want to be.
They only have access to what's been deeply encoded through repetition: the parenting patterns you observed hundreds or thousands of times growing up.
This is why you can know intellectually that yelling doesn't work, be deeply committed to gentle parenting, and still hear your mother's exact words coming out of your mouth when you're overwhelmed.
It's Not About Effort or Intention
Many parents blame themselves for these moments. They think: "I know better. I should be able to control myself. What's wrong with me?"
But this isn't an issue with your effort or your intention, This is a taxed nervous system adapting to extreme stress and change.
When you're well-resourced (rested, supported, within your Window of Tolerance), you can access your prefrontal cortex and parent intentionally. You can pause, choose your response, use the skills you've learned.
When you're depleted (exhausted, at capacity, pushed beyond your window), your brain literally can't access those skills. It's not that you've forgotten them. It's that the part of your brain that houses them has gone temporarily offline.
Understanding this can help reduce the shame spiral that often follows these moments. You're not a bad parent. You're a depleted human whose nervous system responded exactly as nervous systems do under stress.
What Actually Helps
The goal isn't to never have these moments. That's not realistic when you're parenting with a nervous system that's constantly near capacity.
The goal is to:
Notice when it's happening
Understand why it's happening
Repair with your child
Build more capacity over time so these moments happen less often
The most important thing to understand right now is that these moments don't mean you're failing. They mean you're at capacity and need more support.
What do I do with this information?
Understanding matrescence doesn't make the hard moments easier, but it can reduce the shame and self-blame that make everything harder.
When you understand that your nervous system has been rewired, that your capacity has genuinely shrunk, that your stress responses are biological rather than character flaws, you can stop asking "What's wrong with me?" and start asking "What do I need?"
Practical First Steps
1. Notice your Window of Tolerance
Start paying attention to the signs that you're approaching the edge of your window:
Physical tension
Shorter fuse
Difficulty making simple decisions
Wanting to escape or zone out
These aren't character flaws. They're information. Your body is telling you that you're near capacity.
2. Name what's happening
When you feel overwhelmed, try saying (even just to yourself): "My nervous system is at capacity right now. This isn't about me being weak. This is about me being human."
This simple naming can help interrupt the shame spiral and create space for self-compassion.
3. Micro-moments of recovery
You don't always need a spa day. Sometimes you just need:
Three deep breaths before walking in the door
Five minutes sitting in your car after drop-off
Permission to order takeout instead of cooking
A friend who understands "I can't talk, I just need to sit near you"
4. Seek support without shame
If you're consistently feeling overwhelmed, that's not a sign that you're failing at motherhood. It's a sign that you need more support than you currently have.
Support might look like:
Therapy focused on nervous system regulation and parental burnout
Practical help with childcare or household tasks
Medical evaluation if you suspect postpartum depression or anxiety
Community with other parents who understand
In British Columbia, you can find Registered Clinical Counsellors who specialize in perinatal mental health through the BC Association of Clinical Counsellors directory, or access support through the BC Reproductive Mental Health Program.
You're not supposed to do this alone. Our nervous systems evolved for cooperative caregiving, not isolated nuclear families.
The Science Behind Matrescence
The research on maternal brain changes is compelling and helps validate what you're experiencing:
Gray Matter Changes: A landmark 2016 study published in Nature Neuroscience tracked first-time mothers for two years and found significant reductions in gray matter in regions involved in social cognition. These changes were so consistent that researchers could identify which women had given birth based on brain scans alone. Far from being a deficit, these changes represent neural specialization. The brain becoming more efficient at the specific task of mothering.
Amygdala Sensitivity: Research from the National Institutes of Health shows that mothers' brains respond to infant cries within 100 milliseconds. Faster than conscious awareness. This heightened sensitivity persists even when the mother is sleep-deprived, demonstrating how deeply this neurological change is embedded.
Long-term Identity Shift: Anthropologist Dana Raphael first coined the term "matrescence" in the 1970s to describe this profound transition. More recently, reproductive psychiatrist Alexandra Sacks, MD, and researcher Aurélie Athan, PhD, have documented that this transition is comparable in scope to adolescence and involves permanent identity reorganization, not just a temporary adjustment period.
Window of Tolerance: The concept of Window of Tolerance comes from Dr. Dan Siegel's work in interpersonal neurobiology and helps explain why stress tolerance decreases when baseline nervous system activation increases. When you're already operating near the edge of your window just to maintain attunement to your child, there's less room for other stressors.
These aren't just abstract concepts. They're measurable biological realities that explain why you feel the way you do. Understanding the neuroscience doesn't fix the exhaustion, but it can help you stop blaming yourself for a biological process.
Credible Research Links:
Pregnancy leads to structural brain changes (Nature Neuroscience)
Maternal brain response to infant cries (NIH/National Library of Medicine)
Frequently Asked Questions About Matrescence and Maternal Identity
Is matrescence the same as "mom brain"?
No, though they're related. "Mom brain" is often used to describe forgetfulness or difficulty concentrating during pregnancy and postpartum. Matrescence is a much broader concept. It's the entire developmental transition into motherhood that involves structural brain changes, identity reorganization, and nervous system rewiring.
The forgetfulness people call "mom brain" is actually part of the larger matrescence process. Your brain is reorganizing its priorities and using energy for background vigilance and attunement. The executive function required for remembering where you put your keys is being redirected to tracking your child's well-being.
How long does matrescence last?
While the most intense period of brain reorganization happens during pregnancy and the first two years postpartum, many researchers believe matrescence represents a permanent shift in identity and nervous system functioning.
The brain changes documented in research persist for at least two years, and many aspects (like the heightened sensitivity to your child's distress) may last throughout your parenting journey. This doesn't mean you'll always feel overwhelmed, but it does mean you've fundamentally changed. You're not going back to who you were before. You're integrating that person into a new, expanded identity.
Why do I feel angry or rageful instead of sad when I'm overwhelmed?
This is often a "fight" response from your nervous system. When your capacity is exceeded and you tip outside your Window of Tolerance into hyperarousal, your body mobilizes energy to protect you. This often manifests as anger or rage rather than sadness or tears.
Anger feels more energizing than sadness, and when you're already depleted, your nervous system sometimes defaults to the response that gives you a surge of energy. This is especially common when you're experiencing sensory overload. Being touched out, overwhelmed by noise, or bombarded by demands. The rage isn't a character flaw. It's information that your nervous system has hit its limit.
Can my partner experience a version of this?
Yes. While the research on matrescence has focused primarily on mothers (particularly those who carried and gave birth), any primary caregiver can experience brain changes and nervous system shifts through the process of attunement and caregiving.
Partners who are highly involved in caregiving, adoptive parents, and non-gestational parents can all experience increased sensitivity, capacity shrinkage, and identity reorganization. The process may look different without the hormonal and physiological changes of pregnancy, but the nervous system rewiring that comes from being primarily responsible for a child's wellbeing affects anyone in that role.
How can I increase my capacity?
Capacity is increased through what I call "scaffolding." Reducing the sensory and cognitive load in your environment while building in consistent support for nervous system regulation.
This might look like:
Environmental modifications: Reducing visual clutter, creating quiet spaces, minimizing decision fatigue by simplifying routines
Sensory supports: Noise-canceling headphones during overwhelming times, designated touch-free time, reducing screen time when overstimulated
Relational scaffolding: Regular co-regulation with a therapist, partner, or trusted friend; community with other parents who understand
Physiological support: Adequate sleep (when possible), nourishing food, movement that feels good rather than punishing, addressing any underlying health issues
It's important to understand that you can't just "build capacity" through willpower while the demands remain the same. True capacity building requires both increasing your resources AND decreasing the load.
Does having ADHD make matrescence harder?
Yes, significantly. ADHD brains already have differences in executive function, working memory, and sensory processing. When you add the mental load of parenting (the constant task switching, the invisible tracking, the sensory overwhelm) on top of existing ADHD challenges, the nervous system hits capacity much faster.
For ADHD parents, the background vigilance of matrescence is especially demanding because your brain is already working harder to filter sensory input and manage attention. The emotional intensity of your child's big feelings can also be harder to regulate when you have ADHD-related differences in emotional processing.
I've written an entire post specifically about why ADHD makes parenting uniquely challenging and what actually helps. The short version: you need accommodations, not more willpower.
Why does my child's crying feel physically painful to me?
This is your amygdala responding to their distress cue as a physical threat. For some parents, especially those with high sensory sensitivity or a trauma history, their child's crying can trigger a pain response in the body.
This isn't you being dramatic or weak. Research shows that when mothers hear their babies cry, the brain regions associated with both emotional response AND physical sensation activate simultaneously. Your nervous system is interpreting the auditory input as something that requires immediate action to resolve a threat.
If this is happening to you, it's a sign of very high attunement, but it also means you need specific regulation strategies to manage your own response so you can stay present for your child.
How do I repair with my child after I've lost it?
Keep it simple and honest:
"I got overwhelmed and I yelled. That wasn't okay. My big feelings are my responsibility to manage, not yours. I'm working on doing better. You didn't cause my reaction."
Then move forward. Don't over-explain or make your child comfort you. The repair is about taking responsibility and reconnecting, not making them manage your guilt.
Research on attachment shows that repair after rupture actually strengthens the parent-child relationship because it teaches children that mistakes don't break connection and that adults can take responsibility without making kids responsible for their emotions. Your child learns: "People mess up sometimes, and then they come back and make it right. I'm still safe. We're still okay."
Can I be a good mother and still need time away from my children?
Yes. Full stop.
Needing time away from your child doesn't mean you don't love them. It means you're a human with a nervous system that needs recovery time. Your body wasn't designed for 24/7 contact and attunement without breaks.
Think about it this way: You wouldn't expect yourself to work a 24-hour shift without a break and still perform optimally. Why would parenting be any different?
Decompression isn't selfish. It's required maintenance. When you get time to regulate your own nervous system away from the demands of caregiving, you have more capacity to show up for your children when you are with them.
The guilt often comes from cultural messaging that mothers should find complete fulfillment in motherhood and never need anything else. But you're allowed to be a full person with needs beyond your children. Time away allows you to remember who you are outside of "mom." That person deserves care too.
How do I find support for parental burnout in British Columbia?
In British Columbia, look for a Registered Clinical Counsellor (RCC) who specializes in perinatal mental health and nervous system regulation. The BC Association of Clinical Counsellors has a directory where you can search by specialty.
You can also access support through:
The BC Reproductive Mental Health Program (provides consultation and support across BC)
Perinatal Services BC (offers resources and referrals)
Your local public health unit (often has maternal child health programs)
For immediate support, the Postpartum Support International warmline is available at 1-800-944-4773.
When looking for a therapist, you want someone who understands both the psychological aspects of matrescence AND the nervous system/somatic aspects. A clinician who can address both the "why" (attachment patterns, identity shifts) and the "how" (regulation tools, capacity building) will be most helpful.
With over 14 years of experience working with families in Vancouver, British Columbia, I provide this integrated approach. Addressing both the emotional transition and the practical, sensory, and executive function challenges of parenting. If you're in British Columbia and looking for support, I offer both in-person services in Vancouver and online sessions across the province.
What if I think I have postpartum depression, not just matrescence overwhelm?
If you're questioning whether you have postpartum depression, please reach out for assessment. The difference matters because postpartum depression requires specific treatment, not just understanding and support.
Signs that suggest postpartum depression rather than matrescence adjustment:
Persistent hopelessness that doesn't lift with rest or support
Difficulty bonding with your baby or feeling disconnected from them
Intrusive thoughts about harm (to yourself or your baby)
Loss of interest in things you used to enjoy, even when you have the time
Feeling like your family would be better off without you
Physical symptoms like significant changes in appetite or sleep beyond what the baby's schedule creates
In British Columbia, you can:
Talk to your family doctor or midwife about screening
Contact the BC Reproductive Mental Health Program for consultation
Call the Postpartum Support International warmline: 1-800-944-4773
Seek assessment from a Registered Clinical Counsellor who specializes in perinatal mental health
Postpartum depression is highly treatable, and getting help early makes a significant difference. You deserve support, and asking for help is a sign of strength, not weakness.
The Bottom Line
Motherhood rewires your brain in profound ways. Your nervous system becomes more sensitive, your capacity shrinks, and you're asked to function with a completely different biological setup than you had before you became a parent.
The exhaustion you feel, the overwhelm, the moments when you react in ways that surprise you. These aren't signs that you're doing it wrong. They're signs that you're navigating a massive developmental transition with insufficient support and unrealistic cultural expectations.
Your child doesn't need you to have it all together. They need you to be real, to repair when things go sideways, and to show them that being human means having limits.
Give yourself the same grace you'd give your best friend scrolling through those apple orchard photos, wondering what's wrong with her.
Nothing is wrong with you. You're doing something incredibly hard, and you deserve support.
Finding Your Way Forward
If you are reading this and feeling the weight of this transition, please know that you aren't meant to carry this new, expanded nervous system alone. Understanding the "why" behind your overwhelm is the first step toward finding a way through it.
If you’re ready to dig deeper into how this affects your daily life, you might find it helpful to explore why parent burnout isn’t a failure of patience but a sign of diminished capacity, or learn more about how sensory overload and emotional labor can hit ADHD women uniquely hard when routines shift. If you’re currently struggling to bridge the gap with your partner, my post on why vacations and transitions feel so hard when one partner is at capacity offers a nervous-system lens on the mental load. Ultimately, remember that regulation is resilience—it’s not about staying calm all the time, but about having a flexible system that can return to steadiness after the hard moments.
You can find all of these deep dives and practical strategies for your parenting journey at nurturedfoundations.com/blog.
You are doing the brave, exhausting work of becoming. Be as gentle with yourself as you are with your little ones.
Sources & Scientific Review: This post was written with a commitment to evidence-based practice. Key findings are drawn from Nature Neuroscience (Hoekzema et al., 2017) regarding brain plasticity, and the interpersonal neurobiology frameworks of Dr. Dan Siegel. For a full list of clinical citations, [click here to view my references].
Brain Structural Changes (The Landmark Study): Hoekzema, E., Barba-Müller, E., Pozzobon, C., et al. (2017). Pregnancy leads to long-lasting changes in human brain structure. Nature Neuroscience, 20(2), 287–296. https://doi.org/10.1038/nn.4458 > This study confirms the "synaptic pruning" and reduction in gray matter in the social cognition network of first-time mothers.
Amygdala & Response to Infant Cries: Swain, J. E. (2011). The human parental brain: In vivo neurobiological studies of parenting. Neuropsychopharmacology, 36(1), 365–366. https://doi.org/10.1038/npp.2010.138 > This research highlights the rapid activation of the amygdala and emotional processing centers in response to infant stimuli.
The Concept of Matrescence: Athan, A. (n.d.). Matrescence: The Developmental Transition of Motherhood. Columbia University, Teachers College. https://www.matrescence.com/ > Dr. Aurélie Athan is the leading clinical psychologist who revived and expanded the term for modern maternal mental health.
The Window of Tolerance: Siegel, D. J. (2012). The Developing Mind: How Relationships and the Brain Interact to Shape Who We Are (2nd ed.). Guilford Press. > This is the foundational text for the Window of Tolerance concept used in nervous system regulation.
Reproductive Mental Health (BC Specific): BC Reproductive Mental Health Program. (2024). Perinatal Mental Health Care Pathways. Perinatal Services BC. http://www.perinatalservicesbc.ca/